Cna Shower Sheets Template
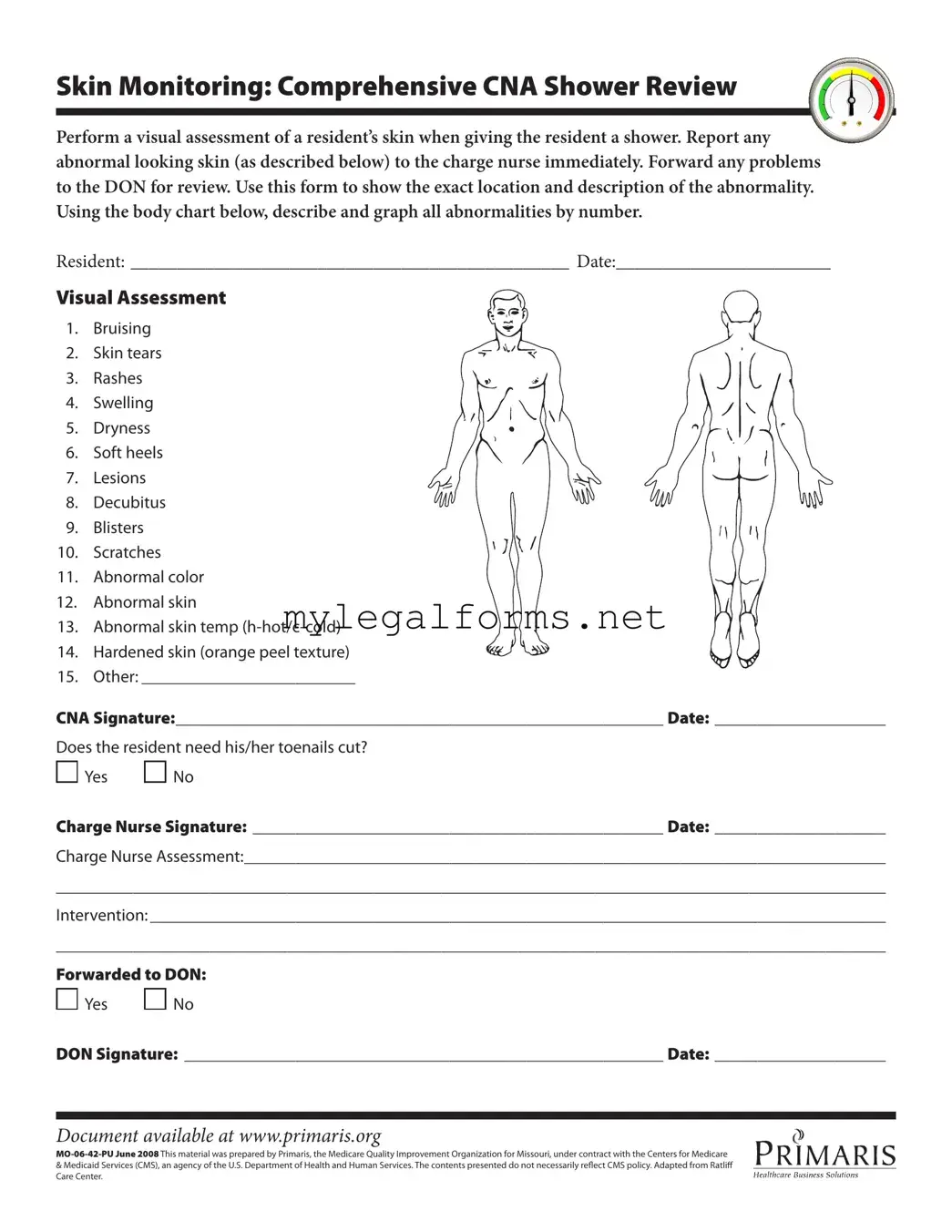
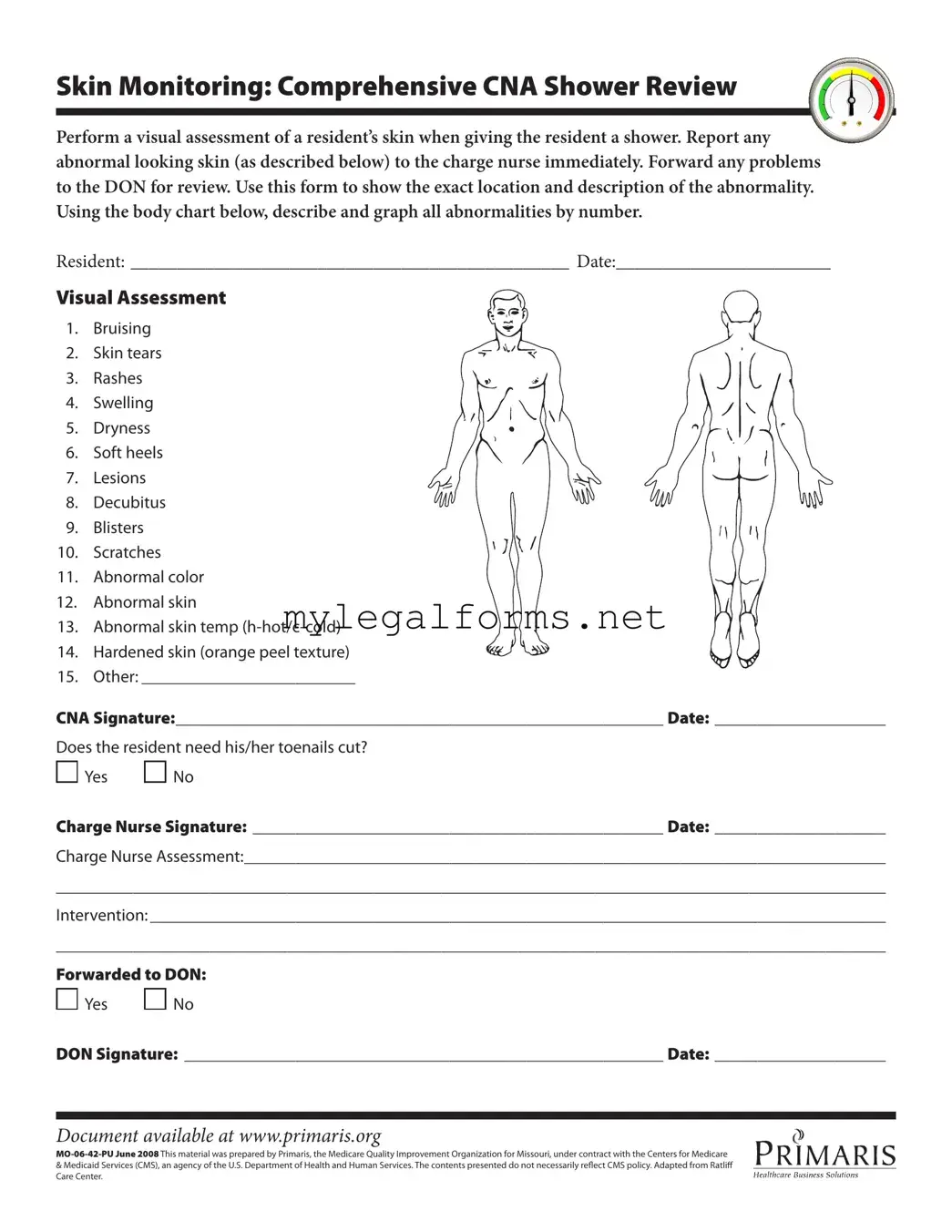
The CNA Shower Sheets form serves as a critical tool for certified nursing assistants to document and assess the skin condition of residents during showers. This form facilitates thorough visual assessments, ensuring that any abnormalities are promptly reported and addressed. By providing a structured way to record findings, it enhances the overall quality of care delivered to residents.
Launch Cna Shower Sheets Editor
Cna Shower Sheets Template
Launch Cna Shower Sheets Editor
Launch Cna Shower Sheets Editor
or
⇓ PDF Form
Complete the form at your pace — fast
Finish your Cna Shower Sheets online and download the final version.

 Yes
Yes 
 No
No
 Yes
Yes 
 No
No