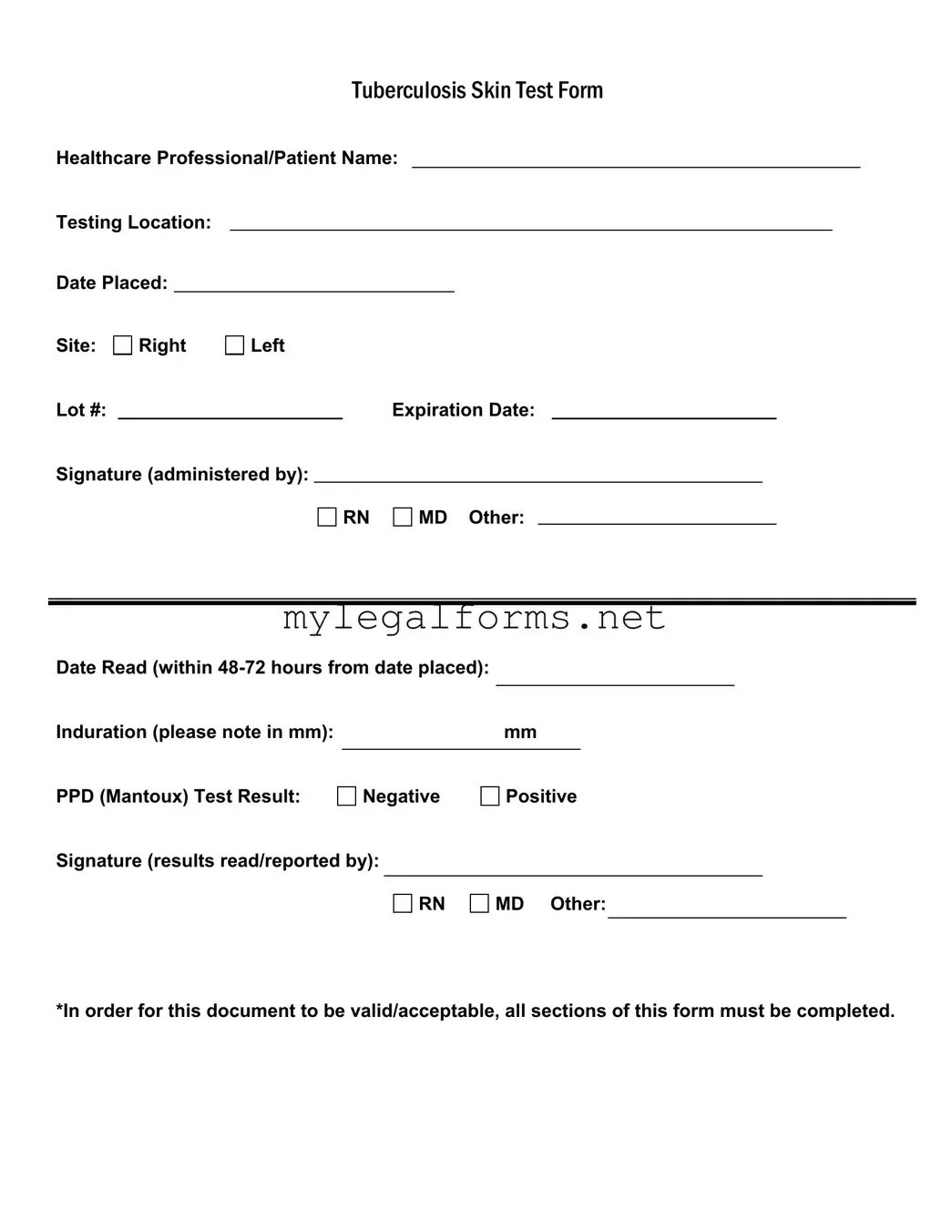
When filling out the Tuberculosis (TB) Test form, individuals often make several common mistakes that can lead to complications or delays in processing. One of the most frequent errors is neglecting to fill in all required sections. The form clearly states that all sections must be completed for it to be valid. Omitting even a single detail can render the form unacceptable, causing frustration and requiring a repeat of the process.
Another mistake involves misplacing the testing location. It is essential to accurately note where the test is administered. An incorrect entry can lead to confusion about where the results should be sent or who is responsible for interpreting them. This can delay important health decisions and follow-up actions.
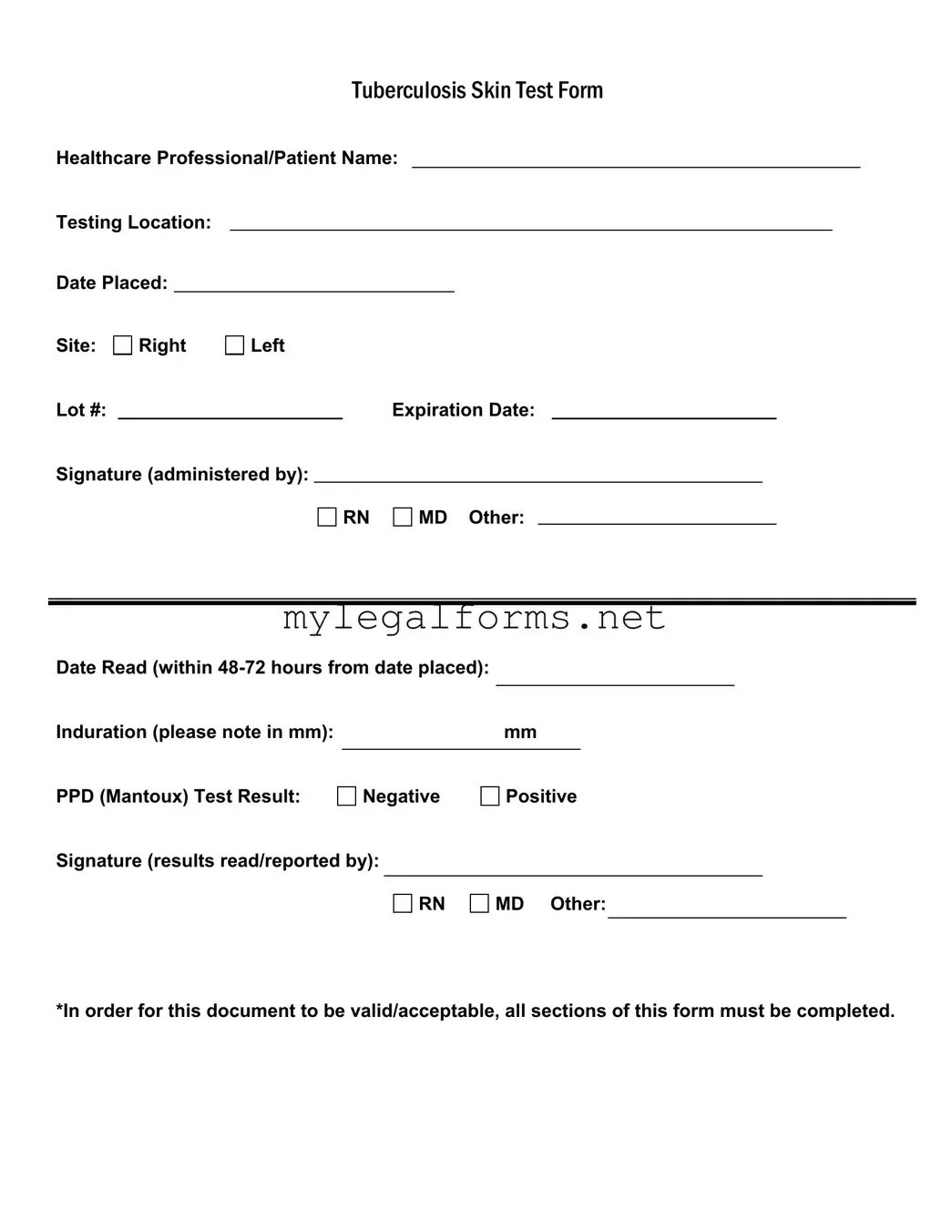
Many people also fail to record the date the test was placed. This date is crucial because it establishes the timeline for reading the results. Without it, healthcare professionals may struggle to determine whether the results are being evaluated within the required 48-72 hour window, which could affect the accuracy of the test results.
Additionally, some individuals mistakenly do not specify the site of the test—whether it was administered on the right or left arm. This detail is vital for both record-keeping and for the healthcare provider to ensure proper follow-up, especially if there are any reactions to the test.
Another common oversight is failing to include the lot number and expiration date of the PPD solution used for the test. These details are important for tracking the efficacy and safety of the test materials. Missing this information can raise questions about the validity of the test results.
When it comes to recording the induration measurement, some people either forget to measure it or misreport the size in millimeters. Accurate measurement is critical, as it determines whether the test result is classified as negative or positive. An error here can lead to misdiagnosis or unnecessary anxiety.
In addition, individuals sometimes overlook the need for a signature from the healthcare professional who administered the test. This signature not only validates the process but also provides accountability. Without it, the form may be considered incomplete, further complicating matters.
Finally, many people do not ensure that the signature of the professional reading the results is included. This signature is essential for confirming that the results have been interpreted correctly. Omitting it can lead to questions about the legitimacy of the findings and may require additional verification.