DEPARTMENT OF HEALTH AND HUMAN SERVICES |
Form Approved |
CENTERS FOR MEDICARE & MEDICAID SERVICES |
OMB No. 0938-0025 |
|
Expires: 04/24 |
REQUEST FOR TERMINATION OF PREMIUM PART A, PART B, OR
PART B IMMUNOSUPPRESSIVE DRUG COVERAGE
WHO CAN USE THIS FORM?
People with Medicare premium Part A or B who would like to terminate their hospital or medical insurance coverage.
WHEN DO YOU USE THIS APPLICATION?
Use this form:
•If you have premium Part A or Part B, but wish to no longer be enrolled.
•If you have Part B, but recently re-joined the workforce with access to employer-sponsored health insurance and wish to voluntarily terminate this coverage.
•If you have Part B, but are now covered under a spouse’s employer-sponsored health insurance and wish to voluntarily terminate this coverage.
WHAT HAPPENS NEXT?
Send your completed and signed application to your local Social Security office. If you have questions, call Social Security at 1-800-772-1213. TTY users should call 1-800-325-0778.
HOW DO YOU GET HELP WITH THIS
APPLICATION?
•Phone: Call Social Security at 1-800-772-1213. TTY users should call 1-800-325-0778.
•En español: Llame a SSA gratis al 1-800-772-1213 y oprima el 2 si desea el servicio en español y espere a que le atienda un agente.
•In person: Your local Social Security office. For an office near you check www.ssa.gov.
WHAT INFORMATION DO YOU NEED TO COMPLETE THIS APPLICATION?
•Your Medicare number
•Your current address and phone number
•A witness and their current address and phone number, if you signed the form with “X”
•Date you are requesting to end your premium Part A or Part B
WHAT ARE THE CONSEQUENCES OF
DISENROLLMENT?
•If you disenroll from Part B, it may result in gaps in your coverage, and you may incur a late enrollment penalty of 10% for each full 12-month period you don’t have Part B but were eligible to sign up and you don’t have other appropriate coverage in place.
•You must have Part B while enrolled in premium Part A. If you disenroll from Part B, your premium Part A will also terminate.
REMINDERS
If you’ve already received your Medicare card, you’ll need to return it to the SSA office or mail it back.
WHAT IF YOU WANT TO RE-ENROLL IN MEDICARE?
If you do not qualify for a special enrollment period (SEP), you will need to wait until the general enrollment period (GEP), which is every year from January—March. Coverage will be effective the month after the month of the enrollment request.
If you would like to re-enroll in premium Part A or Part B you will need to complete the form CMS 18-F-5 or
CMS 40-B. If you qualify for an SEP, youll also need to attach the following:
•If you qualify for an SEP based on employer group health plan coverage, you’ll need to complete the CMS L564.
•If you qualify for an SEP based on another circumstance you’ll need to complete form CMS 10797.
•The forms will need to be provided to SSA per the instructions on each individual form.
You have the right to get Medicare information in an accessible format, like large print, Braille, or audio. You also have the right to file a complaint if you feel you’ve been discriminated against. Visit https://www.medicare.gov/about-us/accessibility-nondiscrimination- notice, or call 1-800-MEDICARE (1-800-633-4227) for more information. TTY users can call 1-877-486-2048.
DEPARTMENT OF HEALTH AND HUMAN SERVICES CENTERS FOR MEDICARE & MEDICAID SERVICES
REQUEST FOR TERMINATION OF PREMIUM PART A, PART B,
OR PART B IMMUNOSUPPRESSIVE DRUG COVERAGE
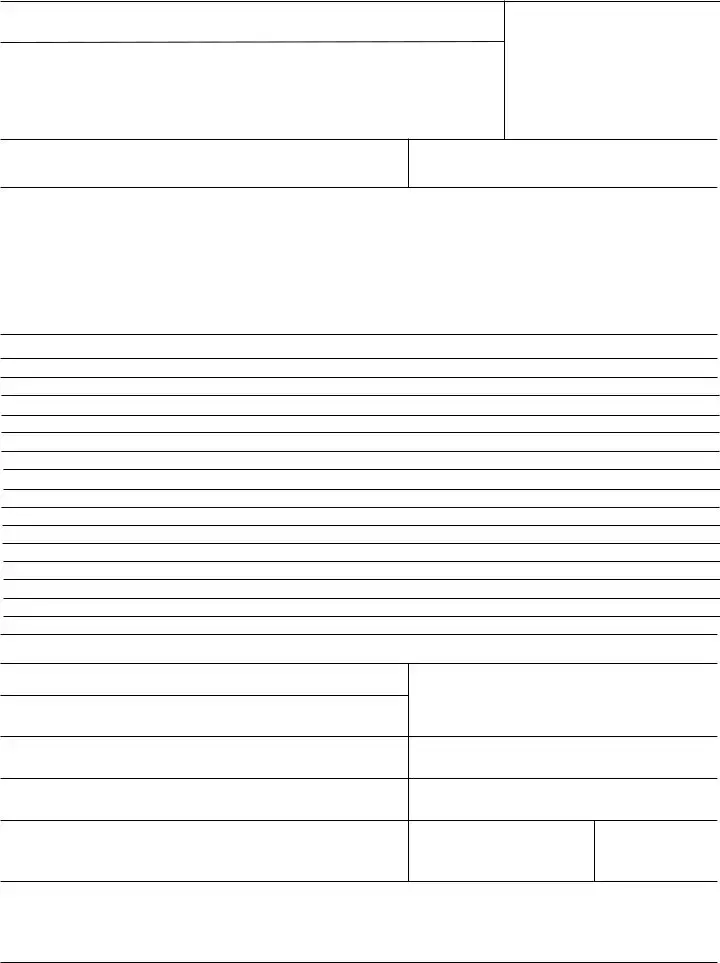
The completion of this form is needed to document your voluntary request for termination of Medicare coverage as permitted under the Code of Federal Regulations. Section 1838(b) and 1818A(c)(2)(B) of the Social Security Act require filing of notice advising the Administration when termination of Medicare coverage is requested. While you are not required to give your reasons for requesting termination, the information given will be used to document your understanding of the effects of your request.
DO NOT WRITE IN THIS SPACE
NAME OF ENROLLEE (Please Print)
NAME OF PERSON, IF OTHER THAN ENROLLEE, WHO IS EXECUTING THIS REQUEST.
THIS IS A REQUEST FOR TERMINATION OF |
DATE PART A |
DATE PART B |
DATE PBID |
HOSPITAL INSURANCE |
WILL END |
WILL END |
WILL END |
MEDICAL INSURANCE |
|
|
|
PART B IMMUNOSUPPRESSIVE DRUG COVERAGE |
|
|
|
|
|
|
|
I request termination of my enrollment under the above sections of title XVIII of the Social Security Act, as amended, for the reason(s) stated below:
I UNDERSTAND THAT IF I AM REQUIRED TO PAY FOR MY HOSPITAL INSURANCE, THE TERMINATION OF MY PART B COVERAGE WILL ALSO END MY PART A COVERAGE.
If this request has been signed by mark (X), two witnesses who know the applicant must sign below, giving their full addresses.
1. NAME OF WITNESS
SIGNATURE (Write in Ink)
SIGN
HERE
ADDRESS (Number and Street, City, State and Zip Code)
MAILING ADDRESS (Number and Street)
ADDRESS (Number and Street, City, State and Zip Code)
DATE (Month, Day and Year)
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0938-0025. The time required to complete this information collection is estimated to average 10 minutes per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have any comments concerning the accuracy of the estimate(s) or suggestions for improving this form, please write to: CMS, Attn: PRA Reports Clearance Officer, 7500 Security Boulevard, Baltimore, Maryland 21244-1850.